The Connection Between Pain and the Brain: The Psychology of Pain Blog Series 1
How do your thoughts and emotions affect your pain? In this exclusive interview, Dr. William Deardorff—a clinical psychologist specializing in pain management—shares his insights.
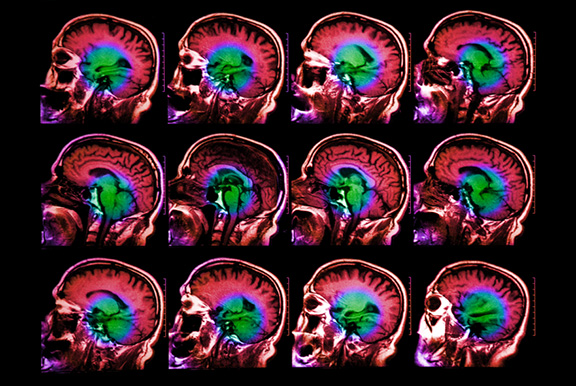
 Dr. Deardorff specializes in the connection between chronic pain and the brain.
Dr. Deardorff specializes in the connection between chronic pain and the brain.See Chronic Pain As a Disease: Why Does It Still Hurt?
Veritas Health:
How did you become interested in the psychological side of chronic pain, and in particular the chronic back and neck pain?
Dr. Deardorff:
I have always been interested in mind-body influences on health.
When I was a psychology intern, I trained with one of the pioneer pain psychologists, Dr. Wilbert Fordyce. While working on his pain rehabilitation unit, I observed amazing results in terms of treatment outcomes.
Chronic back pain patients would come in barely able to walk, taking a lot of pain medicines, and often very depressed.
 Sometimes pain meds are not the answer for patients in chronic pain.
Sometimes pain meds are not the answer for patients in chronic pain.See Medications for Back Pain and Neck Pain
The 19-day inpatient program included intensive exercise, cognitive treatments, relaxation training, sleep stabilization, tapering of pain medications, among other things. In most cases, the results were truly phenomenal. In the program, all the powers of the mind and body were utilized to fight the pain.
The mind-body connection is especially important in the area of chronic back pain. How one thinks about the pain can greatly impact how it is coped with.
Consider a dramatic example that represents a real patient I treated: A woman presented with fairly severe pain in her back, and she was firmly convinced it was due to a cancerous tumor.
 Spine cancer is rare, but the fear of having it can make your pain worse.
Spine cancer is rare, but the fear of having it can make your pain worse.Watch Metastatic Spinal Cancer Video
Her emotional response demonstrated a high level of suffering including fear, depression, and anxiety. Our treatment team obtained an MRI and anatomically her spine was found to be OK. Her pain was real, but it was likely due to a severe muscle sprain/strain and was not life threatening.
Within seconds of getting the news, her emotional response changed dramatically from fear and depression to relief. In this case, the actual pain in her back did not change; the only thing that changed was her belief about the threat of pain and the subsequent emotional response. This illustrates how changing beliefs or thoughts about pain can change a person’s emotional response or level of suffering in response to it.
 Emotional response to pain can have a significant impact.
Emotional response to pain can have a significant impact.Watch: Lower Back Strain Video
The interplay between the mind and body is particularly important in the area of chronic pain, especially back pain. This is why we often see very different pain experiences between patients with the same back injuries or physical findings. Some patients with severe physical problems related to their backs suffer a lot both in terms of the pain and related problems, such as depression, lack of activity, medication side effects, poor sleep, etc. On the other hand, many patients with the same severe physical findings suffer a lot less. Their pain perception might be the same, but their level of suffering in response to the pain is quite different. This response to the pain is where a pain psychologist may help.